CHEST PAIN
Important: Angina can be a warning sign of a heart attack. If you have unexpected or severe chest pain, call 999 right away.
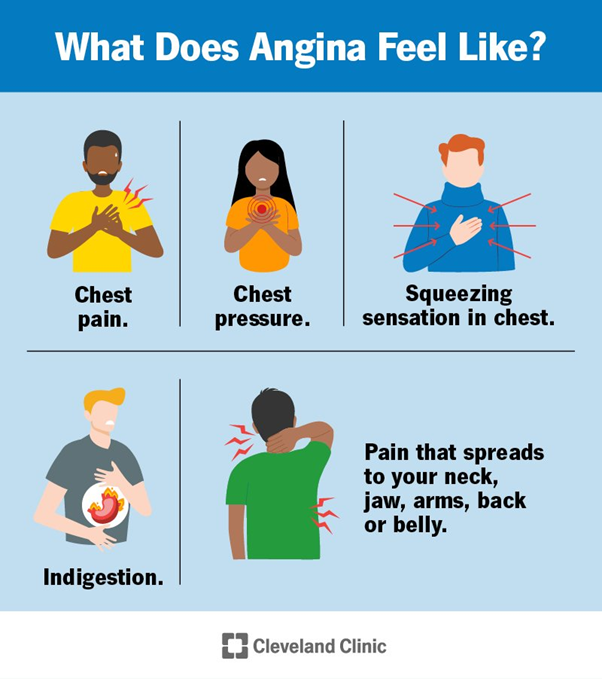
What does angina feel like?
Most people with angina describe having chest pain or pressure. Or they describe a squeezing sensation or a tightness in their chest. Some people say it feels like indigestion. Others say it’s hard to describe angina with words.
The discomfort usually begins behind your breastbone. Sometimes, you may not be able to locate exactly where the pain is coming from.
Pain/discomfort you feel in your chest may spread to other parts of your upper body. These include your neck, jaw, shoulders, arms, back or belly.
Lack of oxygen to your heart can cause other symptoms, known as “angina equivalents.” These are symptoms that you don’t feel in your chest, including:
- Fatigue.
- Nausea or vomiting.
- Shortness of breath.
- Sweating a lot.
- Stable angina.
- Unstable angina.
- Microvascular angina.
- Prinzmetal (variant) angina.
Symptoms of Stable angina:
• Pressure, pain, squeezing or fullness in the center of your chest.
• The feeling may spread to your jaw, neck, back, shoulder or arm.
• May feel like gas or indigestion.
• Lasts five minutes or less.
Symptoms of Unstable angina:
• Pain that feels different from usual stable angina.
• Pain that’s more severe or gets worse.
• May also have shortness of breath.
• May last more than 20 minutes.
• May go away and then return.
Symptoms of Microvascular angina:
• Severe chest pain.
• May also feel shortness of breath, sweating or fatigue or have sleep problems.
• Lasts at least 10 minutes.
Symptoms of Prinzmetal (variant or vasopastic) angina:
• Severe chest pain.
• Vague pain or pressure in your lower chest.
• Pain may spread to your neck, jaw or left shoulder.
• May have cold sweat, nausea, dizziness or fainting.
What is angina pectoris?
Angina pectoris is another name for stable angina. It refers to brief chest pain or discomfort that comes and goes in predictable patterns.
How is angina different from a heart attack?
Both angina and a heart attack are consequences of coronary artery disease. But angina doesn’t cause permanent damage to your heart. A heart attack does. That’s because angina signals a temporary reduction in blood flow to your heart. A heart attack causes a longer reduction in blood flow. During that time, part of your heart muscle begins to die.
Another key difference is what makes the pain go away. Rest or medication (nitroglycerin) causes stable angina to go away within a few minutes. However, if you’re having a heart attack, rest or medication won’t ease your symptoms.
Stable angina doesn’t require emergency care unless your pain suddenly gets worse or doesn’t go away with rest or medication. A heart attack is a life-threatening emergency that needs immediate medical attention. There’s nothing you can do on your own to make it better.
That’s why it’s important to talk with a healthcare provider about your angina and learn what’s “normal” for you. Ask your provider what’s out of the ordinary for you and when you should call 999.
What causes angina?
Reduced blood flow to your heart (myocardial ischemia) causes angina. Several problems with your coronary arteries can prevent your heart from receiving enough blood. These include:
- Coronary artery disease (CAD): This is the most common cause of angina. It happens when plaque (a fatty, waxy substance) builds up in your coronary arteries, which supply blood to your heart. These arteries narrow or harden (atherosclerosis), reducing blood flow to your heart.
- Coronary microvascular disease: This condition is more common among women and people assigned female at birth (AFAB) compared with men and people assigned male at birth (AMAB). It damages the walls of tiny blood vessels that branch from your coronary arteries. These blood vessels aren’t seen on typical testing for CAD and require special testing that’s not available at all medical centers.
- Coronary artery spasm: Your coronary arteries repeatedly constrict (tighten) then open up. These spams temporarily restrict blood flow to your heart. You can have coronary spasms without having coronary artery disease. This may not be diagnosed with routine testing for CAD and may require special testing that’s not available at all medical centers.
There are many risk factors for angina. Some factors raise your risk of heart problems that directly cause angina, like coronary artery disease. Other factors limit how much oxygen-rich blood can reach your heart.
Some risk factors (like aging) are out of your control. You may be able to manage others through lifestyle changes and medications. Talk with your provider about how to lower your risk.
- Anemia (low red blood cells).
- Chronic stress.
- Diabetes.
- Diet high in saturated fat, trans fat, sugar, sodium or refined carbohydrates.
- Drinking too much alcohol.
- Exposure to “particle” air pollution (like dust from roads, farms or construction sites).
- Family history of early heart disease.
- Heart failure.
- Heart valve disease.
- High blood pressure.
- High cholesterol.
- Hypertrophic cardiomyopathy (enlarged heart).
- Inflammation.
- Long-term exposure to secondhand smoke.
- Metabolic syndrome.
- Not moving around enough (physical inactivity).
- Obesity.
- Older age (over 45 for men and people AMAB, over 55 for women and people AFAB).
- Smoking, vaping or using other tobacco products.
- Use of street drugs.
How is angina treated?
Your healthcare provider will treat the underlying heart problem that’s causing your angina. The goals of treatment are to improve blood flow to your heart and lower your risk of complications. Your provider will give you a physical exam and perform testing to learn more about your condition and determine the best treatments.
Common treatment options include:
- Anticoagulants or antiplatelet drugs to lower your risk of blood clots.
- Blood pressure medications.
- >Cholesterol medications.
- Medications used specifically to treat angina.
- Lifestyle changes.
- Coronary artery bypass grafting (CABG).
- Percutaneous coronary intervention (PCI), also called coronary angioplasty and stenting.
Even with treatment, some people still experience angina. Your provider may prescribe a medication to quickly open your blood vessels when you have pain. Nitroglycerin is a common angina medication.
Enhanced external counterpulsation (EECP) is another option for people with continued pain. This therapy applies pressure to your lower legs to help improve blood flow to your heart. It may help ease your angina.
What can I do at home to manage angina?
Talk with your healthcare provider about how to manage angina in your daily life. They’ll offer advice based on the type of angina you have and what’s causing it. Some general tips include:
- Keep a log of your angina episodes. Include the date and time, what it felt like and possible triggers (activities, emotions, weather, etc.). Also include the pain level on a scale of 1 to 10. Share the log with your provider.
- Know when to call for emergency help.
- Take medication as prescribed to treat your angina.
- Try to avoid the triggers that lead to an angina attack.
If you have angina, you may worry about what’ll trigger an angina attack. You may wonder if it’s safe for you to do the following activities:
- Drive.
- Exercise or play a competitive sport.
- Have sex.
- Work a job that involves manual labor.
Talk with your provider about which activities are safe for you. Many people can continue their normal routine, but should keep medicine with them in case of an angina attack. You may need to reduce heavy lifting or other strenuous tasks that could trigger an angina attack. But your provider will offer guidance based on your individual situation.
- Avoid smoking and all tobacco products. Also, avoid exposure to secondhand smoke.
- Eat a heart-healthy diet. The DASH Diet and the Mediterranean Diet are good options. Lower your intake of saturated fat, trans fat, sugar and sodium.
- Find new ways to manage stress. Try meditation, yoga or talking with a counselor or friend. Journal writing is another way to process emotions and concerns.
- Keep a weight that’s healthy for you. Ask your provider what you should aim for, and ask for advice on how to reach that goal.
- Manage risk factors for coronary artery disease. These include high blood pressure, high cholesterol, high triglycerides and diabetes.
- Move around more. Try to exercise for at least 150 minutes (2.5 hours) every week. Go for walks or find other activities you enjoy. Find a friend to join you.
- Take medications prescribed by your cardiologist. Many of these medications have been shown to reduce or eliminate the anginal symptoms you have.
When should I call my healthcare provider?
Call your healthcare provider if you have:
- Questions or concerns about your treatment plan.
- Side effects from your medications.
- Symptoms that are new or getting worse.
When should I go to the ER?
Call 999 or your local emergency number if you have symptoms of a heart attack or stroke. These are life-threatening emergencies that require immediate care. Consider printing out the symptoms so you can keep them visible at all times. Plus, share this information with your loved ones.
You should also call 999 if your stable angina suddenly becomes worse or doesn’t go away with rest or treatment.
Angina is a common symptom of heart disease. Many people can manage their angina by learning their triggers and knowing when to rest or take medication. But sometimes, angina can be a sign of a heart attack. Knowing when to call for emergency help can save your life.
Talk with your provider about your angina. Make sure you know the difference between your “normal” angina and a more severe symptom that needs emergency care.
His presence radiates a warmth, he instils confidence in all those around him, he sets an example for others to follow and is a role model for others to aspire to be like. He was kind, courteous, professional, understanding, caring and highly approachable and relatable as well as the medical guru we all benefit from and rely on to give us our lives back.
In life we all need role models, if I was in training to be a doctor you would certainly fit that role for me. I thank you so much for what you have done to allow me to continue with my fitness regime and wish you well in the life ahead of you.
What I valued as much as his erudition was his people skills, he related to everyone as an individual, his understanding, communications, interactions and personable nature were exceptional. Dr Ubaid was quite simply staggering, he is somebody that has had a significant impact on me, not just for giving me my life back and for his medical genius but for being the person that he is.
Dr Ubaid works well with all the staff. His approach to his fellow workers is both patient and respectful. His easy going manner makes him very approachable to ask advice and he accommodates any delays graciously. I personally look forward to working with him.
Your kindness and good humour were very much appreciated and certainly put me at ease throughout the procedure, which on other ocassions has been quite daunting, your relaxed approach to my problem was very calm and professional.
A great team player, all of the nursing staff are very happy to work with Salahaddin as he is polite, efficient, and has a great aura of calmness and competence and appreciates the time to be light-hearted.
In Dr Salahaddin Ubaid I had a medical genius who also contributed significantly to aiding me overcome all of the negative worries and emotions I was feeling. The care he provided to me, his attention to detail, his personal knowledge, expertise, experience and skills was outstanding.